A dangerous journey to safe hands
The birth of a child is normally a time of joy. But for the most vulnerable families around the world, it can be filled with fear and uncertainty. One mother’s story shows how a lack of adequate maternal and child health care can be devastating for generations of women and children.
By Rita Mu
In remote Kalaki District, in east Uganda, children play in their villages as parents tend to household chores and farming activities.
Dirt roads and paths, spanning across kilometres through bushland, connect homes to schools, health facilities and bustling cities. Some families, if they have enough money, pay for a vehicle to get to these places. For most, however, it is a long and, often, dangerous journey on foot.
For Joyce* and her family it is about a six-hour walk to the nearest health centre. Joyce has made the journey many times – when her babies were sick, and when she was pregnant and in labour.
The first child was a newborn. Joyce had walked close to six hours, fighting through labour pains and contractions, to her nearest health centre to give birth, only to find the facility closed due to a lack of staff and funding. There were no doctors or nurses in sight. Out of time and nowhere else to go, Joyce gave birth on the verandah.
Sadly, her baby died. “The baby didn’t even cry,” Joyce says. “I had no idea what the problem was. If the nurse was present she would have been able to deliver my baby, check and find what the problem was.”
The loss of child, and a mother
A year after losing her baby, Joyce found herself grieving the loss of another child, her 18-year-old daughter Grace*.

“I can’t tell what really happened because she never told us about any unusual pain,” Joyce says. “She was sweating like someone was pouring water on her. We checked and checked on her. She was not breathing.”
Grace did not even get the chance to meet her baby.
It has been almost two years, but Joyce still does not know the cause of Grace’s death.
“If she had reached the hospital the doctors could have figured out what the problem was,” Joyce says.
A huge gap between rich and poor
Stories like Grace’s are all too common in poor, remote communities around the world.
Ninety-four per cent of all maternal deaths around the world occur in low and lower middle-income countries.
Statistics like this highlight the huge gap between rich and poor when it comes to accessing quality maternal health care.
A baby born in Uganda is 11 times more likely to die than a baby born in Australia. For every 1,000 births, 33 infants die in Uganda compared to three infant deaths in Australia.
The difference in maternal death rates between Uganda and Australia is even more staggering. In Uganda, 375 mothers die for every 1,000 births, compared to only six maternal deaths in Australia.
Mothers and babies are dying from complications during, and after, pregnancy and childbirth. Common complications include severe bleeding or infections, high blood pressure during pregnancy, obstructed labour, malaria and heart disease. These complications are often preventable or treatable with the help of a skilled health professional.
However, for mothers and babies living in poverty and remote villages, one of the major barriers to accessing quality maternal and child health care is the long distance they need to travel, usually on foot, to health facilities. Health services are few and far between for families like Joyce’s.
Basic maternal and child healthcare services are often under-resourced and under pressure. The COVID-19 pandemic has further strained these services.
*Names have been changed.
How you can help
Your support can help mothers and babies access the health care they need, and be in safe hands.
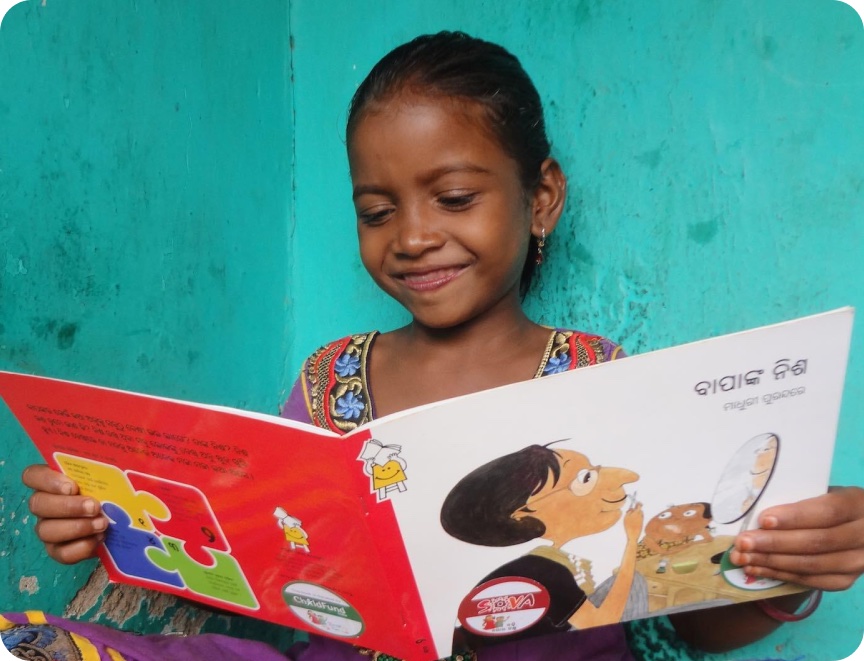
ChildFund is working with local partners and skilled health professionals on the ground in disadvantaged communities to deliver interventions such as:
Health outreach clinics: Skilled health professionals such as nurses at these clinics provide essential services such antenatal care, COVID-19 and child vaccinations, family planning, nutrition assessment of children, and malaria testing and treatment.
Community health volunteers: Trained village-based health volunteers identify and treat common illnesses and diseases such as malaria, which can lead to maternal anaemia, miscarriage, or premature delivery if left untreated. They also connect pregnant mothers with skilled health professionals and antenatal care services.
Birthing kits: Clean birthing kits help pregnant mothers living in remote villages deliver their babies at home more safely if they cannot access a health facility. These kits include the necessary tools and equipment, such as clean sheets, soap, gauze, and a new scalpel and clamps to cut the umbilical cord, for a safer delivery at home.
Medicines and medical supplies: Increased demands for health services and travel restrictions around the globe during the COVID-19 pandemic have led to shortages in essential medicines and medical supplies.
Breaking a multi-generational cycle
No mother should lose a child, and no child should lose their mother during childbirth.

You can help mothers and babies access the health care they need to be in safe hands.